It’s winter, and the UK health service is gearing up for flu season.
Last year, flu and other respiratory diseases caused one third of all excess winter deaths among those over 65. The NHS, facing ever greater pressure, vaccinates thousands against it every year. But there’s a problem.
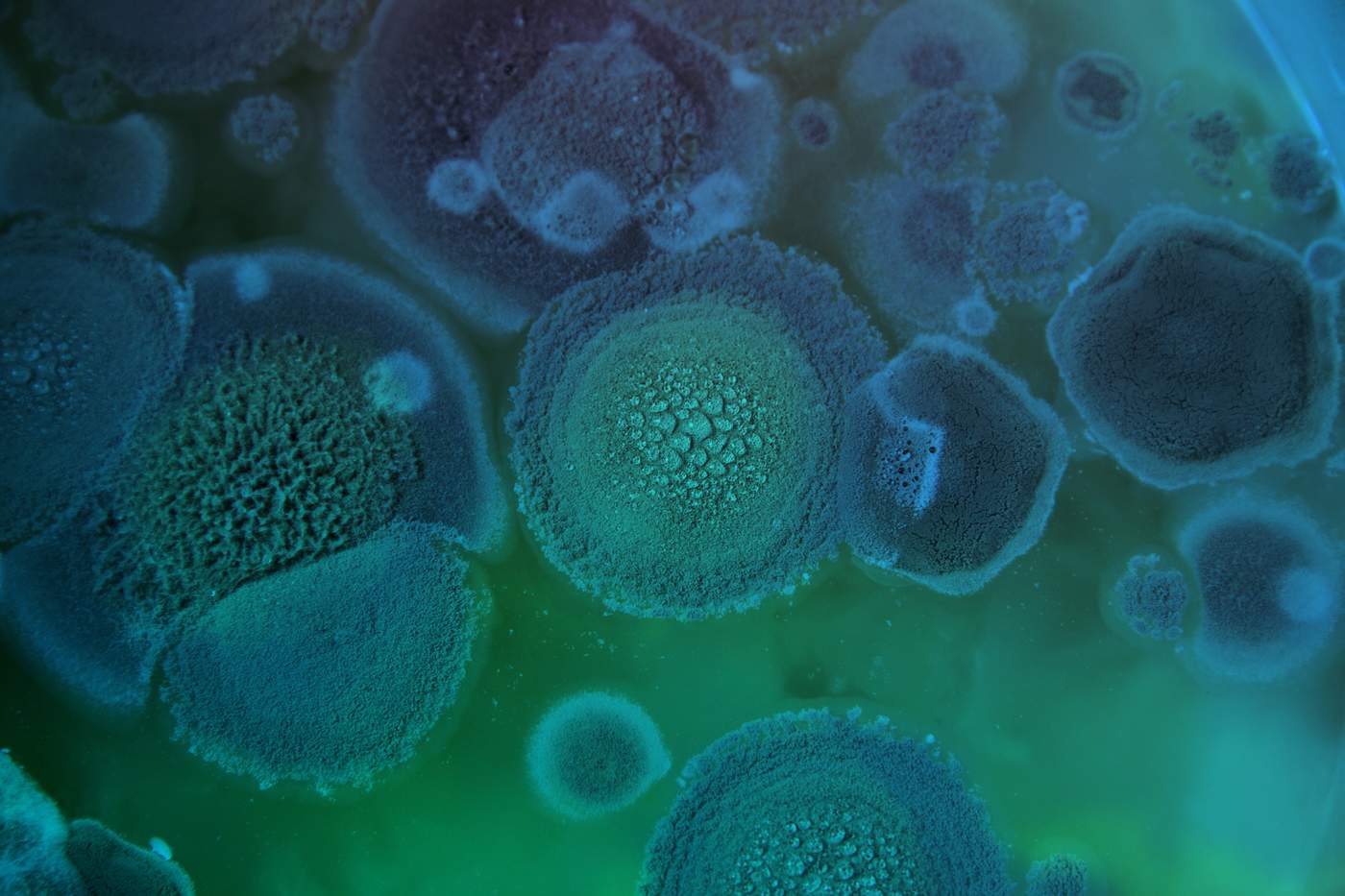
‘As scientists, we know that the current vaccines are flawed,’ says virologist Lynda Coughlan. ‘We need alternatives.’
The Department of Health agrees. Describing the flu vaccine as reaching ‘around 50% (ranging from 25% to 70%) effectiveness’, it cites the virus’ constant mutations as a huge obstacle in protecting vulnerable patients.
Just two flu seasons ago, Dr Coughlan was close to giving up. But now, at the Icahn School of Medicine at Mount Sinai in New York, her research into a universal flu vaccine could be revolutionary. So, what changed?

In the UK, surgeon Shree Datta is preparing a speech on the value of medical research. It’s a topic that's close to her heart.
‘I went into clinical research having been a doctor for about seven years,’ she says. ‘I was used to being on-call, being on the shop floor, moving from ward to ward. So the time out that I took to do research allowed me to pause and catch my breath. It’s a whole different experience.’
Now a consultant obstetrician and gynaecologist, Miss Datta’s research experience – in particular, on a project that investigated new treatments for ovarian cancer – has made a huge impact on her work.
Surgeon Miss Shree Datta discusses her experience of medical research
‘As a clinician, it gave me a different level of understanding about molecular genetics and biology,’ she says. ‘But equally, being able to put forward information to different audiences – scientists, clinicians, patients, members of the public – was a very useful skill for me to develop.’
Today, her research continues – even though she’s long since returned to full-time practice. ‘The group who I work with [were] able to continue the research I kick-started,’ she explains. ‘This could lead to clinical changes to the type of care we provide our patients.’

The problem for fledgling researchers, and for doctors taking their first steps in medical research, is that research funding in the UK can be ‘kind of like the chicken and the egg’, says Miss Datta.
‘Some of the grants I applied to as a junior doctor I wasn’t eligible for because I didn’t come with a wealth of clinical experience,’ she explains. ‘You need to have the experience and expertise behind you so that people put their faith in you.’
For a scientist or clinician at the beginning of their research career, or who wants to move into a new field of research, it can be tough – no matter how good their ideas are. This was the situation facing Dr Coughlan – by now a full-time researcher, but not able to work on her own ideas.
‘If a young researcher wants to try and establish their own thing […] it’s actually really difficult to juggle that with working full time on another project,’ she explains. ‘It’s really challenging. I worked probably seven days a week, 12 hours a day, if not more.
‘I was going into the Jenner Institute [a specialist centre for vaccination development at the University of Oxford] at 7am to set up experiments, going to my other research job at 9am, and coming back to the Jenner Institute at 6pm.

‘In the current climate in the UK, grants are really strict in terms of delivering on the objectives the PI [principal investigator, or lead scientist] has set out,’ she says. ‘The current system is not really ideal for researchers to try and establish independence.’
She applied for fellowships to fund more work on her own ideas. All were rejected, ‘because the topic was a little outside of what my current research expertise was. And unfortunately, [rejections] don’t usually come with a lot of feedback. So it’s very difficult for you to figure out if it’s you personally, if it’s your track record, your CV, your publication list, or if it’s the project.
‘That can be really frustrating. I think a lot of researchers give up at that point. I personally have seen a lot of really talented, fantastic scientists leave research because of the situation being the way it is right now.’
Undeterred, Dr Coughlan applied for a small grant from the University of Oxford.
This secured £10,000 – enough to gather some preliminary data for her project. Then, with the data she’d gathered, she applied for a larger grant from the BMA Foundation for Medical Research.
‘I’d had my eye on [a BMA Foundation grant] for about five years,’ she says. ‘But I was trying to get to the stage where I had an independent project that I thought was novel and different from what other people were doing.’

Around this time, there was another exciting change. Professor Peter Palese – a world-renowned virologist and the first person to build genetic maps for the influenza A, B and C viruses – offered to match her funding and collaborate with her if the funding was granted.
‘I’d actually wanted to work with him for a long time,’ Dr Coughlan says. ‘Then, when I was applying for the BMA Foundation grant, I said, maybe I should contact him. I felt like [his lab, at the Icahn School of Medicine at Mount Sinai] would be a really good place for me.’
‘I hoped I would be lucky,’ she remembers, ‘but I wasn’t holding out any huge hope. I was also applying for other grants as well. The success rate of [most grants] is maybe 10% if you’re lucky. To get one grant, you really need to be applying for a lot.’
But it was good news. ‘I was at the Jenner one morning,’ remembers Dr Coughlan, ‘and I saw the BMA Foundation email. I quite literally cried. I knew it was going to change my life.’
Dr Lynda Coughlan describes finding out about her BMA Foundation grant.
January 2018 will mark a year since Dr Coughlan moved her research to the US.
So far, the project has made great progress. ‘I don’t think I fully appreciated until I came here the real impact [the grant would have],’ she says.
Using data generated with her BMA Foundation funding, she’s secured two more grants, including one for $200,000. She's now building a research team to work with her – two masters students, a post-doctoral researcher and a research assistant. In March 2018, she’s hoping to present data from the project at a conference for the first time.

‘I think one good thing about my project is that it’s quite distinct from what anyone [else] is working on,’ she explains. ‘Scientists are now really beginning to appreciate the real potential for using alternatives such as adenoviral vector vaccines for flu.’
‘And if we could make a universal flu vaccine that could protect against lots of different strains and subtypes of flu, if we could protect people against seasonal flu viruses, as well as emerging viruses like avian flu… if you could reduce annual vaccination programmes to maybe every couple of years – that would have a massive impact on the health system.’
The BMA Foundation, she says, is a fantastic source of support for early-career scientists.
‘Quite often, people have fantastic ideas, [but] at such an early stage that it’s difficult to get funding somewhere else. So you’re essentially giving them the opportunity to develop something completely novel. You’re investing in people, but you’re also investing in new ideas. I think it's fantastic the BMA is investing in this type of research.’
Miss Datta, also a former BMA Foundation grantee, agrees. ‘I know how important the grants can be in supporting young clinicians and more experienced clinicians alike in kick-starting their research careers.’ This has multiple benefits, she says – pushing medical research forward, developing new treatments, and creating expert doctors at the forefront of innovation and change.
‘To put it simply,’ she adds, ‘the funding could influence the type of care that I provide my patients. And that’s invaluable.’
About the BMA Foundation
The BMA Foundation for Medical Research is a not-for-profit funding body, funded solely by legacies and donations. Through it, the BMA supports important, innovative research to advance medicine, medical research and the medical profession.
Apply for BMA Foundation funding
Donate to the BMA Foundation for Medical Research
Credits
Digital producer - Eleanor Dean
Editors - Lisa Hansson, Neil Hallows
Multimedia - Mary-Laine Friday, Matt Saywell
Additional multimedia - Sam Henriques, Tim Dorsch
With thanks to Dr Lynda Coughlan, Miss Shree Datta, the Icahn School of Medicine at Mount Sinai and everyone at the BMA Foundation for Medical Research.